Many of our foreign patients are transferred from abroad, like the boy mentioned in the Growth Period 1, and we also see some patients who are undergoing treatment at another clinic but feel anxious so they seek for a second opinion. One passage in the Hippocratic Oath is "Do not harm," but I sometimes wonder if this is harm rather than treatment. There is a lot to learn, so let's take a look at it together.
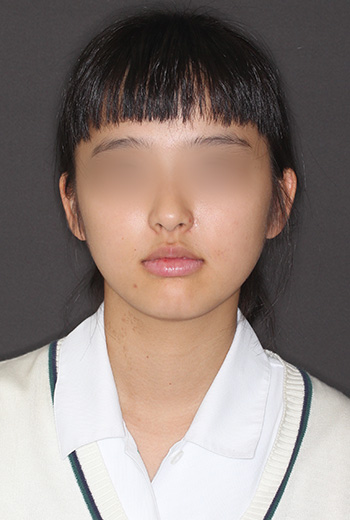
This is a case of a girl who was 11 years and 2 months old at her initial visit. She was wearing appliances to expand the upper and lower teeth laterally, and has already been expanded. I think the goal is to fit all the teeth in, but her bite is unstable. Brackets and wires are attached to the four upper front teeth, but it looks like they are trying to straighten them out. At first glance, they appear to be well-aligned, but the upper left canine has abnormal eruption, and the eruption direction and position are significantly shifted in the alveolar bone, causing root absorption of the upper left central incisor (the tooth in the center of the face). The doctor told her mother that the central incisor needed to be extracted and would be replaced with a dental implant in the future, and she cried, blaming herself for causing great harm to her daughter through treatment she thought it was for her daughter’s own good. I think the mother saw the alignment of her daughter’s front teeth and thought that she needed orthodontic treatment, therefore took her to see the doctor. This is a typical case of orthodontic treatment that only looks at the alignment of the teeth.
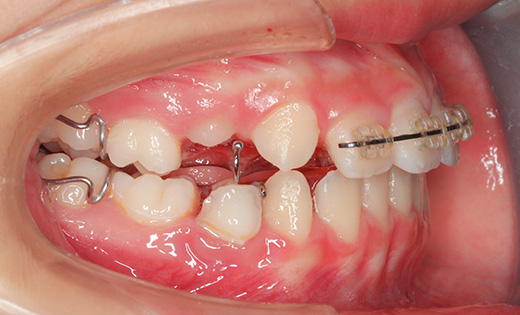

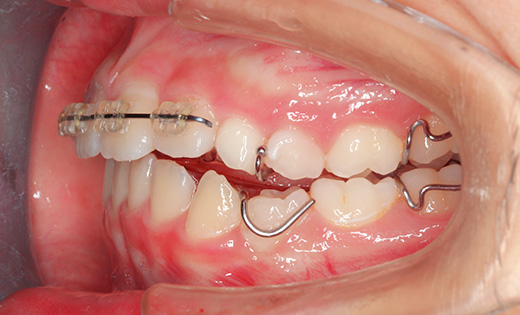
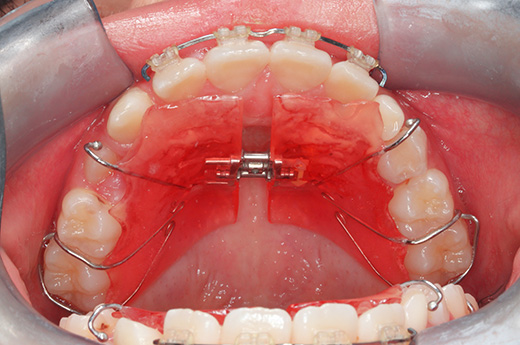

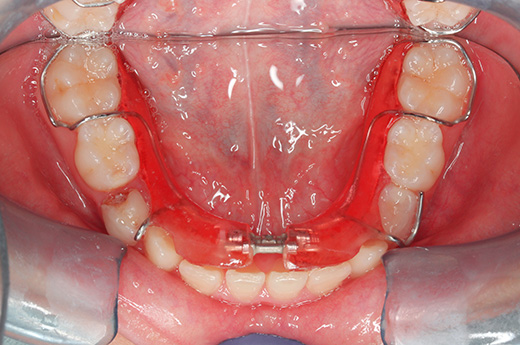
Intraoral photographs at the initial visit. The upper and lower teeth have been fitted with lateral expansion devices, and were already expanded. The bite is unstable. The entire teeth were probably expanded to correct the crooked front teeth. The patient may have been told that expanding them now may avoid the need for tooth extractions in the future. Brackets and wires are attached to the four upper front teeth.

Panoramic X-ray at the initial visit. The upper left canine had abnormal eruption, and the direction and position of eruption in the alveolar bone were significantly shifted, causing root resorption of the upper left central incisor (located in the center of the face). The previous orthodontist must have been shocked to see this photo.
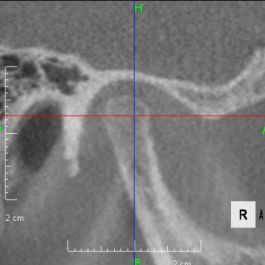
Looking at the CT scan of the Temporomandibular joints(TMJ), the mandibular head has become smaller and deformed in relation to the glenoid fossa. I think the previous doctor did not notice this either. The glenoid fossa has also been deformed flatly, and is not an S-shaped curve like the joint of the boy mentioned in previous case. An MRI scan showed that the articular disc had been deformed downward and forward, and was significantly displaced, with very advanced disc displacement that would not return to its original position even when the mouth was opened. As there are no documents, we do not know the condition before treatment. It is possible that the disc displacement had already progressed before treatment, but I think it is highly likely that the expansion of the dentition caused the bite to become unstable, causing the condition to worsen.
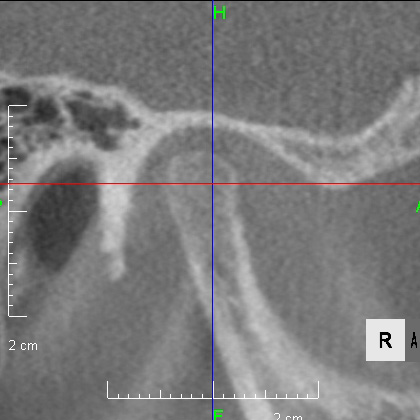
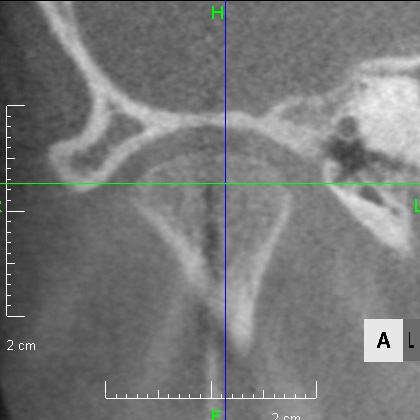
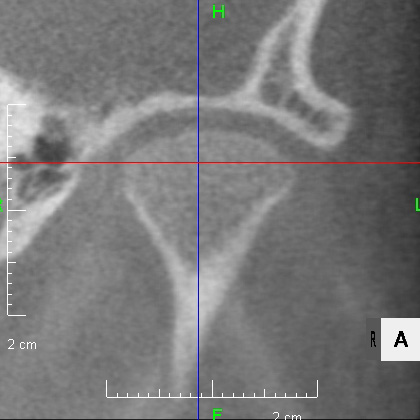
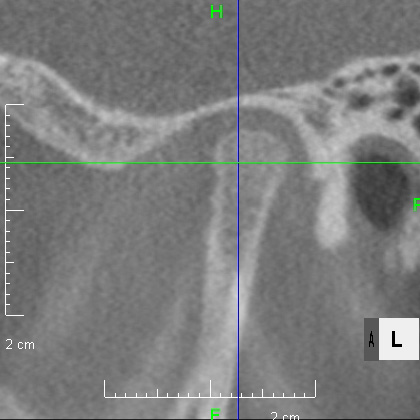
CBCT image of the TMJ at the initial visit. The mandibular head has become smaller and deformed in relation to the glenoid fossa. The glenoid fossa has also become flat and deformed. The CBCT image suggests that the disc may have become dislocated quite a bit.
The problem with this case is that the previous doctor overlooked the abnormal growth and position of the permanent teeth that were about to erupt, and tried to straighten the front teeth without examining the TMJ, resulting in an unstable bite. So what should we do? The disc displacement is at the most advanced stage 4, and there is no going back to the way it was.
Since the root of the upper left central incisor has been absorbed, there is no choice but to extract it. What to do next? The upper left canine, whose root has been eaten, is guided to the position of the central incisor and the direction of eruption is changed.
During this time, the patient had various symptoms such as pain in the TMJ and headaches, so we started with Splint therapy to stabilize the bite at the same time as guiding the tooth position.

The photo on the left is taken immediately after the tooth was extracted. The canine is visible after extraction. The center photo is the extracted central incisor, and the root has been absorbed. The X-ray on the right shows the canine being guided into the position of the extracted central incisor. The canine, which was almost sideways, has changed direction of eruption.

The canine has been guided to the position of the central incisor, and the splint therapy to stabilize the bite, which was performed at the same time, has been completed. The permanent teeth are still erupting, but the root growth of the second molar has progressed by more than half, so it is the perfect time to start orthodontic treatment.






The upper left canine is now in the position of the upper left central incisor, which has been guided. Because the canine and central incisor have different shapes, we used composite to restore the shape, a process called build-up. It is indistinguishable from the central incisor on the opposite side. Treatment to stabilize the bite, which was performed at the same time, prevented the symptoms of the TMJ from worsening any further, and the bite was stabilized in an open bite state.








The photo above was taken at her initial visit when she was 11 years and 1 month old, and the photo below is taken at 12 years and 5 months old. The bite has stabilized, and it was the perfect time to start orthodontic treatment. In both cases, the muscles around the lips are tense when the mouth is closed. After the bite has stabilized, the bite of the teeth inside the mouth is open bite, so the lower facial height from the nose to the chin has become longer. The TMJ had an advanced disc displacement, so there has been very little growth of the lower jaw.
The upper and lower front teeth were protruding, and so were her lips. So we extracted all premolars except the upper left one. While aligning the teeth and facial features, we used the extraction space to rotate the lower jaw counterclockwise to make the chin come forward. Before the orthodontic treatment began, we adjusted the TMJ to create a good environment, but there was no counterclockwise growth of the lower jaw like the boy mentioned in the Growth Period 1. Girls are normally in a growth period from 11 to 12 years old, but unfortunately there was no growth at all in this case where the disc displacement was significant. This case shows that the growth of the lower jaw is affected by the TMJ. We made a treatment plan taking into account that the growth of the lower jaw could not be expected. We started treatment under limited conditions, and the patient understood the situation and cooperated well, so we were able to obtain good treatment results.









At the end of the treatment, she was 15 years and 9 months old. There was no tension around her lips and her facial features were refreshed. Her teeth were also neatly aligned, and we made a comeback from the loss of her central incisors.
The orthodontic device used was an Edgewise Appliance (SWA), and the three premolars except for the upper left one were extracted. The treatment period was two years and 11 months, and the treatment cost was 1,110,000 yen (excluding tax, at that age).
- Commonly cited risks of treatment include root resorption, pulp necrosis, caries development, gingival recession, the onset of TMJ disorder, and worsening periodontal disease, but in this case the TMJ disorder condition improved.
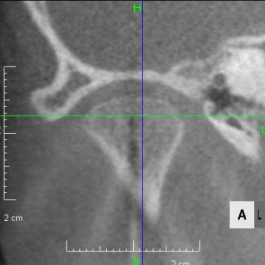

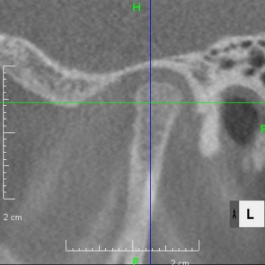
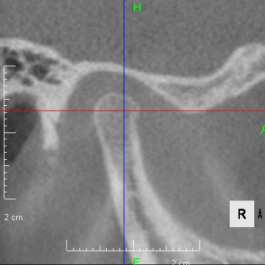
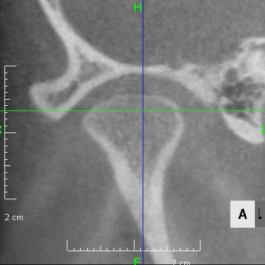
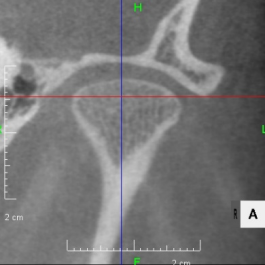
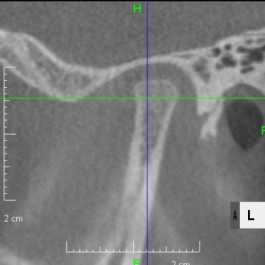
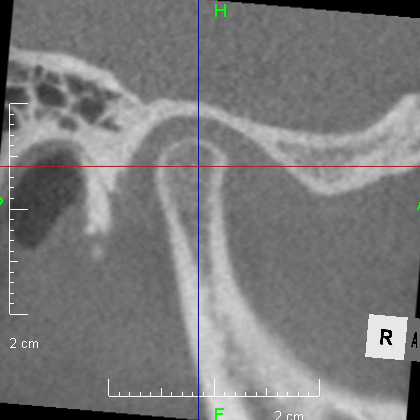
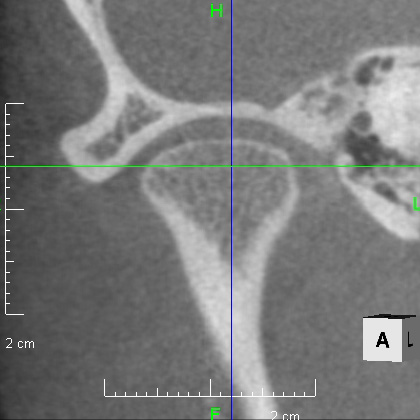
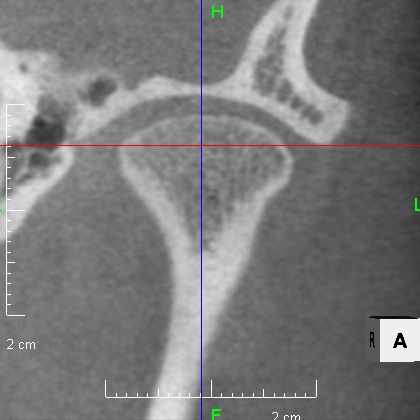
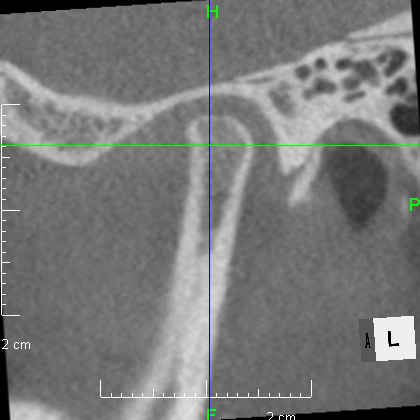
From above, a comparison of CBCT images of the TMJ at the initial consultation, at the start of orthodontic treatment, and at the end of treatment. The mandibular condyle has become smaller and deformed in relation to the glenoid fossa. The glenoid fossa has also become flattened. By taking care to maintain the stability of the bite during orthodontic treatment, there was no further deformation of the mandibular condyle or glenoid fossa, and the shape of the mandibular condyle has become rounded and smooth, providing good function.
To summarize this case, we can see that an unstable lower jaw has a negative effect on its growth. Unfortunately, there was no growth at all in the period when the most growth should occur according to age. This also reminds us of the importance of diagnosis before orthodontic treatment. It is important to diagnose correctly and provide appropriate treatment when necessary. In this case, too, the cooperation of the patient was a great help in achieving success.
